Overview
Difficulty swallowing (dysphagia) comprises problems that usually fall into two categories:
- Oropharyngeal dysphagia — related to nerve and muscle problems that can weaken your throat muscles and make it difficult to move food from your mouth into your throat.
- Esophageal dysphagia — referring to the sensation of food sticking or getting hung up in the swallowing tube (esophagus).
Diagnosis
Diagnosis of dysphagia begins with a thorough review of your medical history and a physical exam. Specialists in digestive diseases, ear, nose and throat (ENT), speech-language pathology, and occupational therapy may be involved in your evaluation.
Oropharyngeal dysphagia
Among the tests used to diagnose mouth and throat (oropharyngeal) dysphagia are:
- Modified barium swallow (videofluoroscopic swallow study). A video X-ray shows the mouth, throat and swallowing tube (esophagus) as you swallow a variety of liquids and food mixed with a metallic liquid called barium.
- Fiber-optic endoscopic swallowing evaluation. Your ability to swallow, as well as the sensation in your throat, is evaluated using a special camera (endoscope) and lighted tube.
- Imaging tests. Computerized tomography (CT) or magnetic resonance imaging (MRI) scans.
Esophageal dysphagia
The following tests may be ordered to look for blockage (obstruction), irritation and motility problems in the swallowing tube (esophagus), and whether the esophagus is pumping too hard or not enough.
- Barium swallow (esophagram). A video X-ray is used to view movement of liquids and food (mixed with a metallic liquid, barium) through the esophagus when you swallow.
- Endoscopy. Your doctor examines your throat and esophagus with a flexible, narrow tube (endoscope) inserted into your mouth and down the esophagus.
- Esophageal manometry. A small tube (catheter) is used to measure esophageal pressure and record the duration and sequence of muscle contractions.
- pH probe. A thin tube is passed into the esophagus to determine if stomach acids are entering your esophagus (acid reflux).
- Imaging scans. If esophageal cancer is suspected, your doctor may order a computerized tomography (CT) scan, endoscopy, endoscopic ultrasound or positron emission tomography (PET) scan.
Treatment
Dysphagia caused by gastroesophageal reflux disease (GERD) is usually treated with medications.
Swallowing difficulties caused by motility disorders (esophageal muscle squeezing) may be treated by:
- Stretching narrowed passages with dilation
- Inserting a metal or plastic tube (stent)
- Injecting onabotulinumtoxinA (Botox) in the lower portion of the esophagus
Some severe swallowing problems require a feeding tube that bypasses the mouth and throat.
Surgery
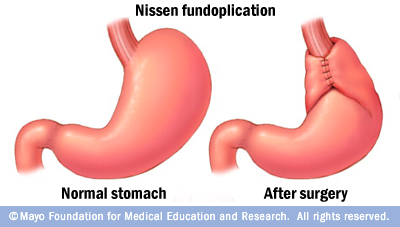
Fundoplication surgery helps relieve acid reflux for people with GERD.
Surgery may be recommended to relieve swallowing problems caused by throat narrowing or blockages, including bony outgrowths, vocal cord paralysis, gastroesophageal reflux disease and achalasia, or to treat esophageal cancer. Speech and swallowing therapy is usually helpful after surgery.
- Laparoscopic Nissen fundoplication involves tightening the lower esophageal sphincter, a muscular valve at the end of the esophagus, to prevent acid reflux in people with gastroesophageal reflux disease (GERD).
- Laparoscopic Heller myotomy is used to cut the muscle at the lower end of the esophagus (sphincter) when it fails to open and release food into the stomach in people who have achalasia. Surgeons at Mayo Clinic are able to perform this with minimally invasive surgery, reducing your recovery time.
- Laryngeal suspension surgery. When swallowing therapy is not helpful in treating dysphagia due to vocal cord paralysis, the voice box can be lifted (suspended) with a surgical procedure to improve swallowing abilities.

